Suboxone® vs. Methadone: What’s the Difference and Which is Best for You?
Opioid use disorder (OUD) deeply affects individuals, families, and communities worldwide. This condition, characterized by a problematic pattern of opioid use, takes a severe toll on the human brain, altering its chemistry and function in ways that fuel dependence and complicate recovery efforts.
In 2019 alone, drug use resulted in 600,000 deaths globally, with nearly 80% of those deaths linked to opioids, and a quarter directly caused by opioid overdose. Unfortunately, this crisis only continues to worsen. Compared to 1999, the number of overdose deaths was ten times higher in 2021. This alarming trend and continued rise in opioid-related fatalities highlight the urgent need for effective treatment and recovery strategies.
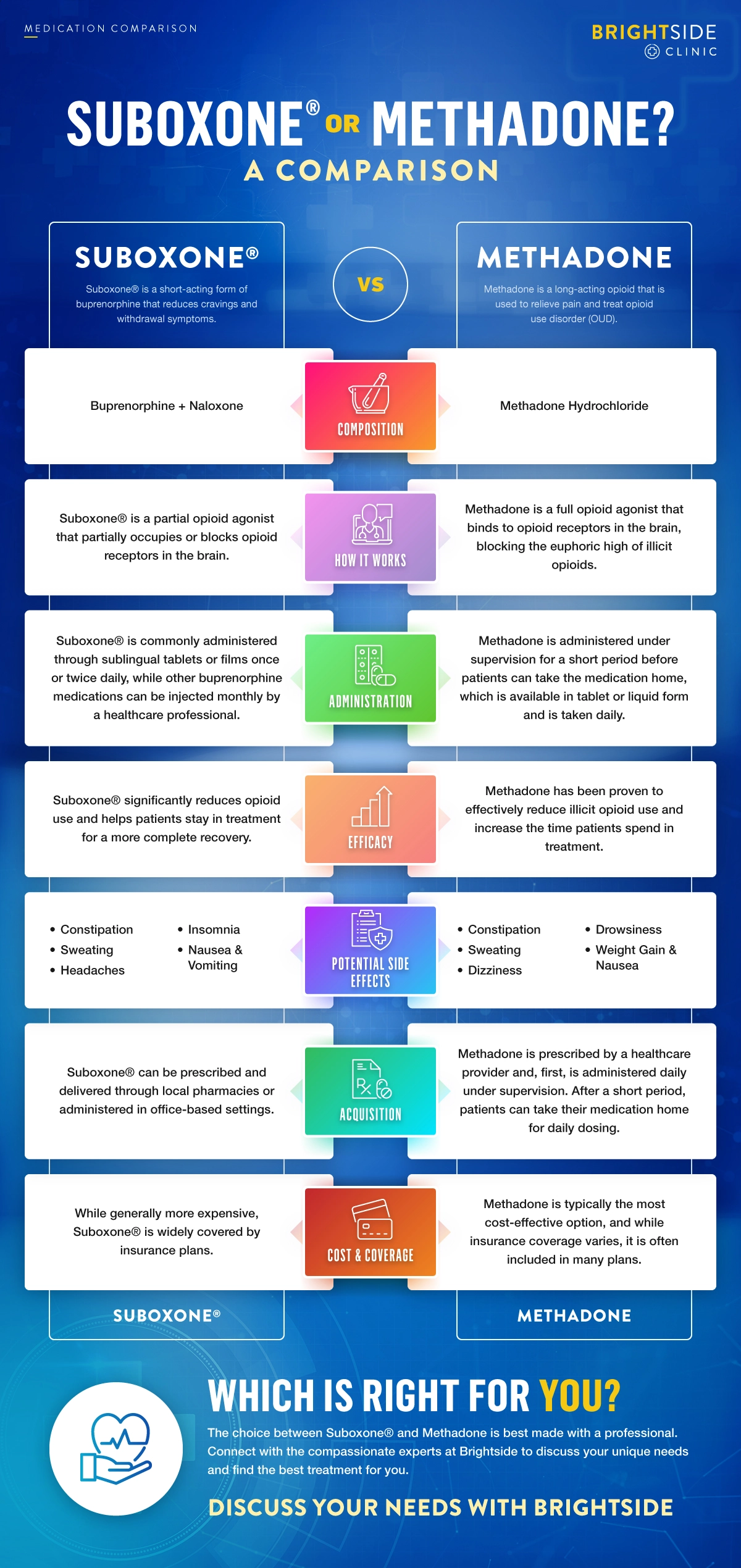
Medication-assisted treatment (MAT) has emerged as a beacon of hope in this escalating crisis. Among the variety of medications available, Suboxone® (a combination of buprenorphine and naloxone) and Methadone are two standard options, each offering a unique treatment pathway. But what is the difference between these two medications, and how do you determine the best choice for your situation? Continue reading to learn more about these treatments and discover the best option for your recovery.

Get Treatment Now
What is Medication-Assisted Treatment?
Medication-assisted treatment (MAT) is a comprehensive approach to treating opioid use disorder (OUD), offering a blend of scientific innovation and compassionate care. MAT integrates the use of FDA-approved medications with counseling and behavioral therapies. This dual-focus strategy aims to treat the physical aspects of OUD while also addressing the underlying psychological and behavioral aspects of the disorder, facilitating a more rounded and sustainable recovery process.
The medications used in MAT are specifically designed to reduce cravings and withdrawal symptoms. These medications work on the same opioid receptors in the brain as the abused opioids, but in a controlled and safe manner, helping to restore balance and begin the recovery process. The Food and Drug Administration (FDA) has approved several medications for use in MAT, including:
Buprenorphine:
Available under brand names such as Brixadi®, Sublocade®, Suboxone®, and Zubsolv®, buprenorphine is a partial opioid agonist. It binds to opioid receptors in the brain without producing the full opioid effect, helping to alleviate withdrawal symptoms and cravings without the high opioid misuse provides.
Methadone:
As a full opioid agonist, Methadone works by binding to the same brain receptors as other opioids, but it does so more gradually without causing the euphoria of drugs like heroin. It helps patients manage long-term withdrawal symptoms and is administered under strict supervision by a practitioner.
Naltrexone:
Used in brand-name drugs such as Vivitrol®, naltrexone is an opioid antagonist, blocking the effects of opioids at the receptor sites in the brain. Naltrexone is mainly used to prevent relapse rather than manage withdrawal symptoms and is suitable for patients already detoxified. This medication is available as a pill or as a monthly injection.
Understanding Suboxone®
Suboxone® is a formulation of buprenorphine, a short-acting partial opioid agonist that is taken once or three times daily. By partially activating opioid receptors in the brain, buprenorphine reduces cravings and withdrawal symptoms without producing the intense high or harmful side effects that come with opioid abuse. With Suboxone®, patients can focus on their recovery journey with a clearer mind and a reduced risk of relapse.
The effectiveness of Suboxone® is enhanced by its combination with naloxone, an opioid antagonist. Naloxone is primarily a safety feature, as it is inactive when Suboxone® is taken as prescribed, under the tongue or inside the cheek. However, if the Suboxone® is injected, the naloxone will activate and block opioid effects and deter misuse.
Suboxone® has four strengths, catering to the needs of patients at different stages of their recovery journey. These strengths include:
- 2 mg buprenorphine/0.5 mg naloxone
- 4 mg buprenorphine/1 mg naloxone
- 8 mg buprenorphine/2 mg naloxone
- 12 mg buprenorphine/3 mg naloxone
Each dose typically works for about 4 hours, but because buprenorphine has a long half-life, it stays in the system for approximately 37 hours. This long half-life contributes to a stable level of medication in the bloodstream, ensuring withdrawal symptoms and cravings are effectively managed with one or two daily doses.
For patients looking for a less frequent dosing schedule, long-acting injections such as Brixadi® and Sublocade® are an effective alternative. These formulations of buprenorphine typically last for a month, simplifying the treatment process and ensuring treatment is easily accessible, regardless of a busy schedule.
The Benefits and Risks of Suboxone® Treatment
Suboxone® is a beacon of hope for those struggling with OUD, providing a pathway toward recovery that is effective and manageable. Suboxone® is designed to offer several key benefits, including:
- Reduced Opioid Use and Misuse Potential: Suboxone®’s unique medical properties reduce the desire for opioids and alleviate cravings without the euphoric high of abused opioids, helping patients lower their use and avoid the cycle of misuse or relapse.
- Eliminated Withdrawal Symptoms: One of the most significant barriers to recovery from opioid addiction is the fear of withdrawal. Suboxone® effectively minimizes withdrawal symptoms, making the process more comfortable and less intimidating for patients.
- Extended Treatment Time: The long-acting nature of buprenorphine allows for extended stability between doses, contributing to a more sustained and stable treatment experience. Additionally, many facilities will not require counseling when on Suboxone, reducing the time spent in the clinic during treatment.
However, Suboxone® is not without its risks. Some of the risks of Suboxone® treatment include:
- Dependence: Although Suboxone® is designed to reduce the risk of opioid misuse, there is still a chance that patients develop a dependence on the medication. However, this risk is significantly lower than with other opioids.
- Withdrawal: If Suboxone® treatment is suddenly stopped, patients may experience withdrawal symptoms. Any changes in dosage or discontinuation of the medication should be done under the guidance of a healthcare provider.
- Liver Damage: There is a risk of liver damage associated with Suboxone®, especially for those who consume alcohol while using the medication. Regular monitoring or liver function tests are recommended to identify and address potential issues early in treatment.
- Side Effects: Like all medications, Suboxone® can cause side effects, including nausea, vomiting, dizziness, and headaches. Although these side effects are generally mild and temporary, they should be discussed with a healthcare provider if they persist.
How is Suboxone® Administered?
Suboxone® is available in different formats, allowing patients to choose their preferred administration method. The sublingual film form is the most common. It is designed to be placed under the tongue, dissolving quickly and allowing the medication to be absorbed through the mouth’s membranes directly into the bloodstream. This method ensures that the active ingredients begin to work quickly, reducing cravings and withdrawal symptoms.
For those who may benefit from a less frequent dosing schedule, Suboxone® can be replaced with a buprenorphine injection such as Brixadi® or Sublocade®. These injections are long-acting forms of buprenorphine that provide a steady level of medication over an extended period. Buprenorphine injections are administered by a healthcare provider in a clinic. They are particularly beneficial for patients who need the convenience of monthly treatment rather than daily medication.
A doctor must prescribe Suboxone® and its generic brands. The prescription will specify the dosage and whether the patient should take their dose once or twice daily, depending on their treatment needs and the doctor’s requirements. This personalized approach ensures that each patient receives the optimal dosage to manage their condition effectively.
Understanding Methadone
Methadone is a long-acting opioid that alleviates pain and facilitates recovery from opioid use disorder (OUD). It binds to the same receptors in the brain as other opioids but doesn’t release the euphoric high that comes with other substances. With methadone, patients gradually wean off more harmful opioids and reduce their dependence while mitigating withdrawal symptoms and cravings.
Available in tablet and liquid forms, Methadone can meet patients’ unique preferences and medical needs. Its long-lasting effects, typically up to 24 hours, provide steady and continuous relief from withdrawal symptoms. This extended duration supports a once-daily dosing schedule that simplifies the process and helps stabilize patients in treatment.
The Advantages and Risk Factors for Methadone Treatment
Methadone treatment offers a range of benefits designed to enhance recovery and quality of life for those navigating the path to sobriety. Some of these advantages include:
- Improved Chance of Long-Term Recovery: By providing a stable, controlled level of opioid agonist treatment, Methadone helps individuals maintain their commitment to recovery, significantly improving their chance of long-term success.
- Reduced Misuse or Relapse Potential: Methadone reduces the euphoric effects associated with opioid misuse, lowering the temptation to relapse. Its long-acting properties also mean that patients don’t experience the highs and lows that can trigger relapse, offering a smoother recovery journey.
- Minimized Withdrawal Symptoms and Cravings: Methadone effectively mitigates the difficulties of managing withdrawal symptoms and cravings, making it easier for individuals to focus on their recovery without the constant battle against physical and psychological urges.
While Methadone treatment offers substantial benefits, there are also risks to be aware of throughout the treatment process. These include:
- Abuse/Dependence Potential: As a Schedule II controlled substance, Methadone carries a risk for abuse and dependence. Its opioid agonist properties can lead to misuse, mainly if a healthcare professional does not closely supervise treatment.
- Long Withdrawal Periods: Transitioning off Methadone can be challenging due to its long-acting nature, which causes the medication to remain in the system for extended periods. Withdrawal symptoms may last longer, requiring a carefully managed tapering process to minimize discomfort.
- Potential Side Effects: Patients may experience side effects such as drowsiness, nausea, vomiting, dizziness, and sweating. While these are typically manageable, they can affect quality of life. They should be discussed with a healthcare provider if they occur.
- Counseling Services: Unlike Suboxone®, most facilities that administer Methadone require the patient to participate in counseling services as part of the treatment process. This holistic approach ensures that the psychological aspects of addiction are addressed. Methadone patients must commit to a comprehensive treatment program with more regular clinic visits.
How is Methadone Administered?
Initially, Methadone must be administered under close supervision to ensure that the dosage is effective and safe. Patients receive Methadone from a practitioner in a clinic or healthcare facility. The supervised setting allows healthcare providers to assess the patient’s response to the medication, adjust dosages as needed, and provide support and counseling.
Over time, as patients stabilize on their dose and adhere to their treatment plan, they may be able to take their medication home between clinic visits. This offers more flexibility and normalcy in daily life but also comes with increased responsibility for managing medication. Methadone is typically taken once per day due to its 24-hour effects, helping patients maintain consistent medication levels in the body to keep withdrawal symptoms and cravings at bay. Methadone is available in both tablet and liquid forms, providing options to accommodate patient preferences and specific medical requirements.
The duration of Methadone treatment varies depending on the patient’s unique needs and progress. A minimum treatment time of 12 months is generally recommended to ensure the best chance of long-term recovery. Extended treatment periods may be necessary, however, as Methadone is often a critical component of a long-term management strategy for OUD.
Comparing Suboxone® and Methadone: What’s the Difference?
Suboxone® and Methadone are both FDA-approved medications used for managing opioid use disorder (OUD), yet despite their shared goal of aiding recovery, these medications have significant differences that influence treatment decisions, including the length of treatment, medication availability, and overall approach to managing addiction.
Suboxone® can be prescribed in specialized substance abuse programs or by a general practitioner with specific training monthly, either in person or via telehealth appointment. This wider availability makes it easier for patients to acquire Suboxone® and begin their treatment journey.
Higher insurance costs and self-dosing may be a barrier to Suboxone® entry for some. On the other hand, Methadone is typically administered through specialized clinics that patients must visit daily for their dose, especially at the start of treatment. This schedule can be more restrictive for patients but allows professionals to closely monitor their reaction to the medication and ensure they adhere to the treatment plan.
One of the most significant differences between these two medications is their potential for abuse and withdrawal time. Methadone, being a full opioid agonist, has a higher potential for abuse than Suboxone®. Because Suboxone® includes naloxone, an opioid antagonist that is activated when the medication is not taken as prescribed, the abuse potential is reduced. However, both medications require a carefully managed tapering process to mitigate withdrawal symptoms when discontinuing use, with Methadone generally associated with more extended withdrawal periods due to its long-acting nature.
Choosing the Right Medication for Treating Opioid Use Disorder
Navigating the path to recovery when struggling with opioid use disorder involves making informed decisions about the most suitable medication-assisted treatment options. With Suboxone® and Methadone offering practical solutions for managing OUD, the question isn’t about which treatment is universally “better,” but which is the best fit for your needs. Several factors influence this decision:
- Severity of Addiction: The intensity of your opioid dependency plays a crucial role in determining the most appropriate medication. Some individuals may respond better to Suboxone®, while others may find Methadone’s effects more suited to their level of dependency.
- Medical History: Your overall health, including any existing medical conditions and medications, may affect the effectiveness of Suboxone® or Methadone. These factors can influence how the body metabolizes the medication and the potential for adverse interactions.
- Lifestyle Considerations: The practical aspects of your daily life, including work schedules and family responsibilities, might sway your preference towards a medication that offers more flexibility or requires less frequent dosing.
- Health Insurance Coverage: The extent of your health insurance coverage could also play a significant role in your decision-making process, as some plans may cover one medication more extensively. Typically, Methadone is more fully covered by insurance than Suboxone®.
Consulting with a Brightside expert is essential when determining which medication is best for you. Our compassionate team members are equipped to assess your unique situation, including your lifestyle, budget, and specific treatment needs, to provide an MAT recommendation that aligns with your personal recovery goals and maximizes your chance of a successful outcome.
Remembering that MAT should not be completed in isolation is also essential. MAT should be used in conjunction with counseling and therapy to address the root cause of addiction. This comprehensive approach ensures that both the physiological and psychological aspects of addiction are treated. A Brightside expert can guide you through this integrated treatment process, creating a plan that encompasses medical and therapeutic support tailored to your needs.
Access Life-Changing Treatment at Brightside
When working to overcome opioid use disorder, understanding the available treatment options is essential. Suboxone® and Methadone are both effective options for managing OUD, offering hope and recovery support for many individuals. Suboxone® is known for its accessibility and safety profile, catering to those who might benefit from a treatment that general practitioners and specialists can prescribe. Methadone, on the other hand, offers a different approach with its long-acting formula, providing stable, day-long relief from cravings and withdrawal symptoms.
Brightside Clinics understands that the battle against addiction is deeply personal, and there is no one-size-fits-all solution. That’s why our experts are dedicated to creating tailored treatment plans that meet each patient’s unique needs, addressing all facets of addiction. Our comprehensive approach ensures that you receive medication-assisted treatment alongside the counseling and therapy you need to tackle the root causes of addiction.
If you or someone you love is navigating life with OUD, we encourage you to reach out to our compassionate professionals. By scheduling a telehealth visit with Brightside, you can discuss your needs and discover how we can support you on your path to recovery. Together, we can find a treatment plan that aligns with your lifestyle, goals, and journey toward a brighter, substance-free future.